Identify Reimbursement Risk Before Claim Submission
By the time most denials are identified, the patient is discharged and the opportunity to fix documentation is gone.
RevProtect shifts your teams from reactive recovery to proactive prevention.
Predict Adverse Payment Outcomes Before Claims are Submitted
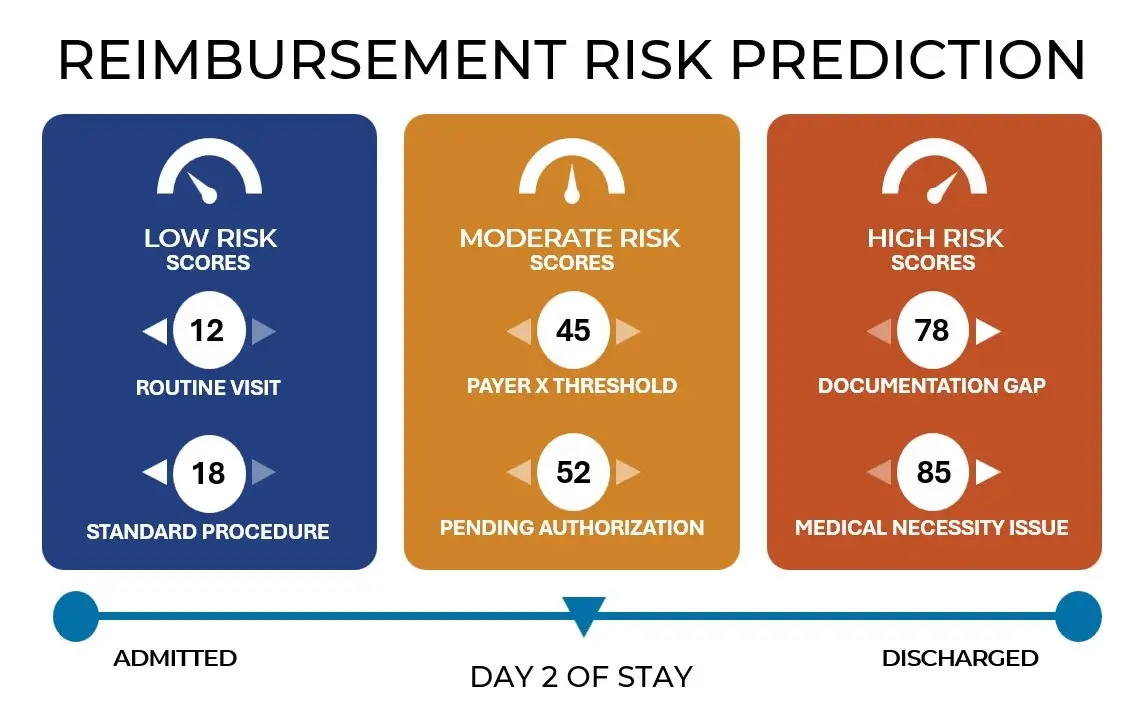
RevProtect predicts the likelihood of adverse payment outcomes at the case level, modeling reimbursement risk as clinical documentation evolves—not after a claim is denied.
By continuously aggregating clinical, 837, and 835 data, RevProtect analyzes both the adequacy of clinical evidence and the probability of triggering payer-specific business rules. This highlights which cases are at risk, why they’re at risk, and where intervention will matter most.
The Revenue Risks RevProtect Identifies
RevProtect reveals reimbursement risk across multiple adverse payment outcomes.
These predictions update continuously as documentation, coding, and utilization data change. Teams can intervene while outcomes are still influenceable.
Payer-specific Reimbursement Intelligence
RevProtect learns and models the unique adjudication behavior of individual payers.
Instead of applying generic rules or static denial logic, RevProtect analyzes historical denial, downgrade, and payment outcomes. This enables RevProtect to identify specific documentation requirements, thresholds, and business rules required by each payer.
This payer-specific intelligence distinguishes between:
- Documentation that is clinically sufficient but payer-insufficient
- DRGs that are defensible with one payer but high risk with another
- Cases where additional evidence will materially change the outcome
RevProtect learns these payer-specific patterns over time and applies them at the individual claim level so teams understand what’s missing and what matters for the payer who will adjudicate the claim
Same case, different payer expectations
For a pneumonia with pleurisy case (DRG 193-195):
Payer A
May approve DRG 193-195 with standard documentation: Chest X-ray with infiltrate, including location and pattern, clinical features supporting diagnosis, and auscultation findings.
Payer B
Requires additional pleurisy-specific documentation: Evidence of pleuritic chest pain, pleural rub on auscultation, documentation of pleural effusion characteristics (reactive vs. parapneumonic).
Payer C
Demands comprehensive treatment response validation, which includes all requirements from Payers A and B plus: Defervescence timeline, clinical improvement markers, transition to oral medications and resolution of leukocytosis.
From Prediction to Action
RevProtect’s payer insights inform and improve RevProtect’s actionable recommendations, guiding documentation improvement, utilization review, coding decisions, and appeal strategies.
This connection between prediction and action helps health systems reduce avoidable denials, protect case mix index, and improve clean claim rates across diverse payer portfolios.
Aligned to Outcomes, Not Promises
RevProtect is available through a performance-based engagement model designed to align incentives and reduce risk. Sift partners directly with health systems to tie success to measured reductions in denials and adverse payment outcomes (not activity, licenses, or usage). If RevProtect doesn’t deliver real, objective impact, clients don’t pay.
Talk with us about whether a performance-based model makes sense for your organization.
