Predictable Reimbursement.
Protected Revenue.
Payer rules are constantly changing. RevProtect applies advanced AI to ensure health systems capture every dollar they’ve earned.
Prevent Revenue Loss
RevProtect delivers payment intelligence that predicts, prevents, and resolves reimbursement risk for health systems turning clinical and payments data into next-best actions across UR, CDI, Coding, and PFS.
Why Reimbursement Has Become Harder
- Payers use AI to scrutinize documentation and downgrade claims, including retrospective audits on claims that were paid 12+ months ago
- Revenue loss now happens through various adverse payment outcomes: level-of-care downgrades, denials, clinical validation or DRG reductions and takebacks
- Revenue risk is introduced before billing, not just at denial
- Teams are understaffed and overworked
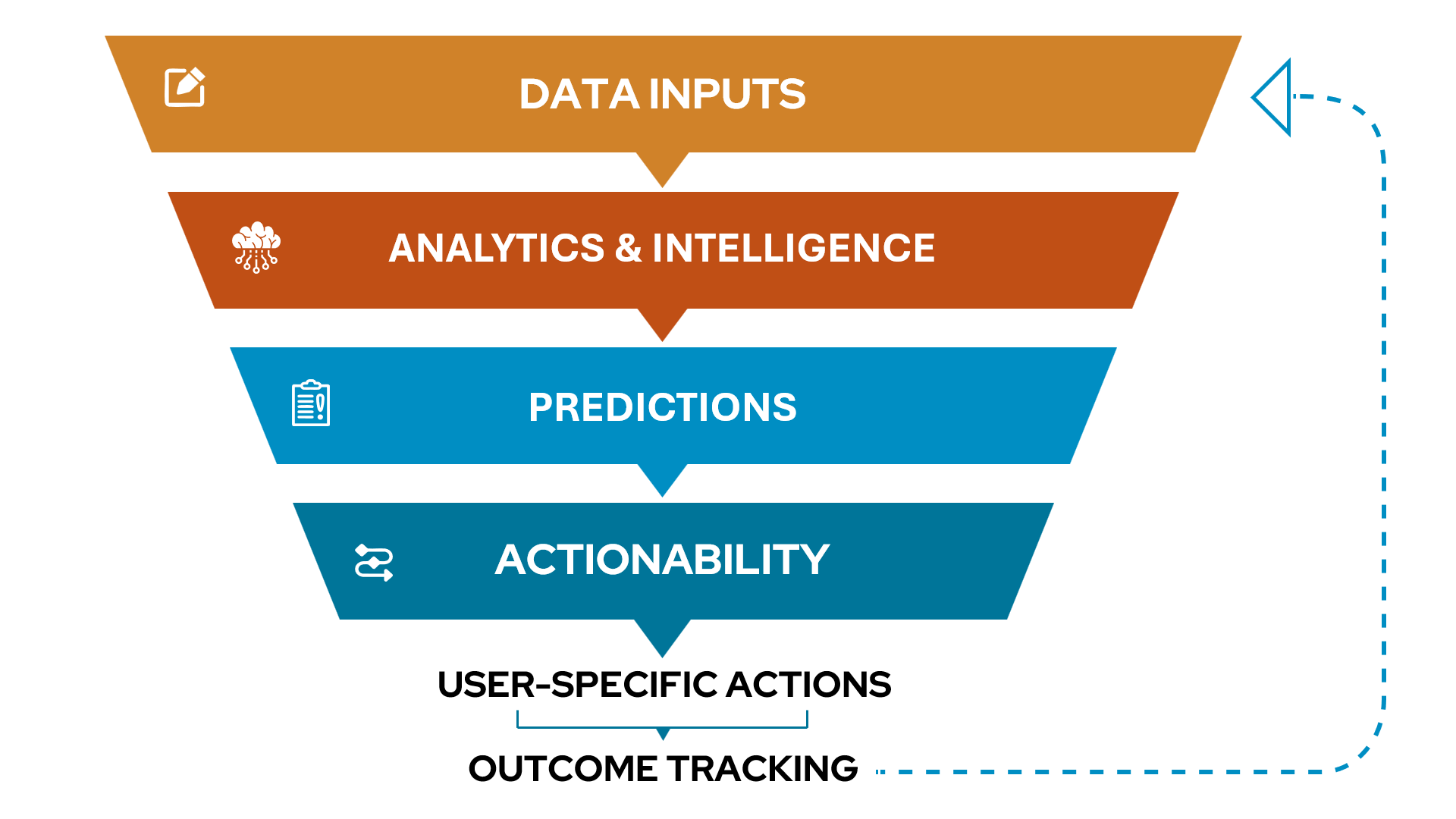
RevProtect addresses these challenges through four integrated capabilities:
Real, Impactful Savings.
For a representative $1B health system:
Enterprise-Grade Data Foundation
coverage
adoption
How Health Systems Deploy RevProtect
RevProtect is designed to fit into existing revenue cycle workflows, reducing portal friction, improving adoption, and making lift measurable from day one. Choose the deployment path that matches your environment:
Use Sift’s UI
Get value fast with a purpose-built experience for denials, overturnability, and prevention workflows.
Embed in existing tools (EHR or third-party)
Bring predictions, recommendations, and rationale directly into the worklists and queues teams already live in, with adoption and throughput lift tracked at the user and workflow level.
Work through a partner
Deploy through one of Sift’s strategic partners to accelerate integration and scale across your footprint.
Real-World Results
$3.9 Additional Revenue Capture in 12 months via downgrade prevention and automated appeals
*Illustrative; varies by payer mix, denial rates, and workflow adoption.
Sift Intelligence
Get in Touch
Prevent costly denials while making your CDI, coding, and UR workflows more efficient and connected.

